Feeling constantly hungry, battling random cravings, or feeling like your body is “working against you” is not a personal failing. GLP-1, a key hormone that regulates appetite, fullness, and blood sugar, plays an important role in these experiences.
It is released from intestinal L-cells after eating and helps stimulate insulin, reduce glucagon, slow stomach emptying, and promote satiety, making it central to metabolic health and a major target in obesity and type 2 diabetes care.
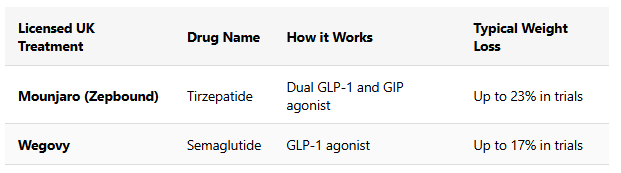
Medications like semaglutide and tirzepatide are designed to mimic or enhance GLP-1 activity, but everyday dietary choices can also help support your body’s own GLP-1 response.
Research suggests that people with higher natural GLP-1 responses may eat around 20–30% fewer calories after a meal, highlighting how powerful this hormone can be in shaping appetite. The following article focuses on six food categories rich in specific nutrients that may naturally stimulate GLP-1 release and help you feel more satisfied throughout the day.
Six Everyday Foods That May Naturally Boost GLP-1 Levels
Supporting your body’s natural GLP-1 response may be simpler than many people expect. Below are six food categories that research has linked with GLP-1 activity, along with practical ways they are commonly included in everyday diets.
Eggs
Starting the day with eggs is a common dietary choice in many balanced eating patterns. Eggs provide a source of high-quality protein and fats, nutrients that have been studied for their potential role in supporting feelings of fullness after meals.
Some research suggests that meals higher in protein, including those containing eggs, may be associated with improved post-meal blood sugar responses and increased satiety when compared with higher-carbohydrate breakfasts. These effects are thought to involve appetite-regulating hormones such as GLP-1 and peptide YY (PYY), which play a role in signalling fullness.
Including eggs as part of breakfast may help some people feel more satisfied for longer and support overall dietary balance. As with all foods, individual responses can vary, and eggs are best consumed as part of a varied, nutritious diet.
Certain Types of Nuts
Nuts such as almonds, pistachios, and peanuts provide a combination of protein, unsaturated fats, and dietary fibre that slows gastric emptying, supports insulin sensitivity, and is associated with increased GLP-1 release and satiety.
Regular nut intake has been linked with improved glycaemic control, greater fullness, and reduced risk markers for type 2 diabetes and cardiovascular disease in clinical and epidemiological studies.
Fermentation of nut fibre by gut bacteria produces short-chain fatty acids, which can stimulate GLP-1 secretion from intestinal L-cells through dedicated receptors and related metabolic pathways.
If you are not allergic to nuts, include a small handful of nuts as a snack or add them to meals like yoghurt, salads, or porridge as a practical way to support natural GLP-1 activity and promote fullness. Evidence suggests that nut-based snacks can enhance satiety and modulate appetite-regulating hormones, including GLP-1, compared with refined-carbohydrate options.
High Fibre Grains
Whole grains such as oats, barley, and whole wheat are rich in soluble fibre, which helps smooth out post-meal rises in blood glucose and is associated with increased GLP-1 secretion and improved satiety. Soluble fibre forms a gel-like texture in the gut that slows digestion and glucose absorption, providing a more gradual stimulus for appetite-regulating hormones like GLP-1 and PYY.
A key part of this effect comes from fermentation of fibre by gut bacteria into short-chain fatty acids (SCFAs) such as acetate, propionate, and butyrate, which can activate receptors on intestinal L-cells and promote GLP-1 release. Randomised controlled trials have shown that high-fibre, oat-based meals can increase GLP-1 and PYY levels, enhance fullness, and reduce subsequent energy intake compared with low-fibre cereals.
Choosing high-fibre grains like oats and barley in place of refined grains (for example, white bread or sugary cereals) is a practical, research-supported way to support natural GLP-1 activity and appetite regulation. People with coeliac disease or gluten intolerance should select certified gluten-free whole-grain options and seek personalised dietary advice where needed.
Avocado
Avocado is a source of monounsaturated fats and soluble fibre, nutrients that are commonly associated with supporting satiety and digestive comfort. Soluble fibre can contribute to slower digestion and more gradual nutrient absorption, while unsaturated fats are often included in dietary patterns linked with metabolic health.
Some research has explored the relationship between avocado consumption and post-meal hormonal responses, including appetite-regulating hormones such as GLP-1 and peptide YY (PYY). These studies suggest that meals containing avocado may be associated with greater feelings of fullness and more stable post-meal insulin responses in some individuals.
Including avocado in meals such as salads or sandwiches may help support satiety as part of a balanced diet. Individual responses can vary, and avocado is best consumed alongside a variety of other nutrient-rich foods.
Olive Oil
Olive oil is a key component of Mediterranean-style eating patterns and is a source of monounsaturated and polyunsaturated fats. Diets that include higher proportions of unsaturated fats are commonly associated with cardiometabolic health and may influence post-meal satiety responses.
Research examining Mediterranean dietary patterns has explored their relationship with appetite-regulating hormones, including GLP-1. Some studies suggest that meals rich in unsaturated fats, such as those containing olive oil, may be associated with differences in post-meal hormonal responses and markers of glycaemic control when compared with lower-fat dietary approaches. These effects are thought to involve interactions between dietary fats and gut-derived hormones, although the exact mechanisms are still being studied.
Using olive oil in cooking or as a salad dressing can be a practical way to include unsaturated fats as part of a balanced diet. As with all dietary choices, individual responses may vary, and olive oil is best consumed in moderation alongside a variety of nutrient-rich foods.
Vegetables
Non-starchy vegetables such as Brussels sprouts, broccoli, and carrots provide dietary fibre, vitamins, and a range of plant compounds that support overall nutritional quality. Fibre-rich foods are commonly associated with digestive health and may influence feelings of fullness after meals.
Some research has examined how the order in which foods are consumed -such as eating vegetables before carbohydrate-rich foods-may affect post-meal glucose responses and appetite-related hormones, including GLP-1. These studies suggest that prioritising vegetables earlier in a meal may be associated with more gradual rises in blood glucose and differences in satiety signals, particularly in certain populations. The underlying mechanisms are still being explored and may involve interactions between dietary fibre, digestion, and gut-derived signals.
Including non-starchy vegetables as part of the first course of a meal can be a practical way to increase fibre intake and support balanced blood sugar responses as part of an overall healthy eating pattern. Individual responses may vary.
How Food May Actually Trigger GLP-1?
The secretion of GLP-1 is closely linked to nutrient sensing by L-cells in the distal small intestine and colon. Specific nutrients, including proteins, peptides, fatty acids, and monosaccharides, interact with G-protein coupled receptors and transporters on L-cells, triggering intracellular signalling cascades that culminate in GLP-1 exocytosis.
Protein ingestion, for example, leads to the generation of peptides and amino acids that bind to calcium-sensing receptors and other nutrient sensors on L-cells, directly stimulating GLP-1 release. Similarly, mono- and polyunsaturated fats activate free fatty acid receptors (FFAR1 and FFAR4), while fibre-derived SCFAs interact with FFAR2 and FFAR3 to promote GLP-1 secretion.
Overall, protein, healthy fats, and dietary fibre represent the three main dietary triggers for endogenous GLP-1 release. Their combined presence in whole, minimally processed foods accounts for the satiety-enhancing and glucose-lowering effects observed in dietary intervention studies.
Fibre and Gut Health Synergy
The interplay between dietary fibre, gut microbiota, and GLP-1 secretion exemplifies the complex synergy underlying metabolic health. Fibre that escapes digestion in the upper gastrointestinal tract is fermented by colonic bacteria, resulting in the production of SCFAs such as acetate, propionate, and butyrate. These SCFAs serve as signalling molecules that activate FFAR2 and FFAR3 on L-cells, directly inducing GLP-1 release.
This gut microbiota-mediated mechanism not only enhances GLP-1 secretion but also confers additional metabolic benefits, including improved insulin sensitivity, reduced inflammation, and maintenance of gut barrier integrity. The inclusion of high-fibre foods such as whole grains, nuts, vegetables, and legumes thus represents a cornerstone of dietary strategies aimed at boosting GLP-1 and supporting overall metabolic health.
Conclusion
Dietary patterns that include adequate protein, fibre, and unsaturated fats are commonly associated with satiety, balanced blood sugar responses, and overall metabolic health. Foods such as eggs, nuts, high-fibre grains, avocado, olive oil, and non-starchy vegetables provide a range of nutrients that have been studied for their potential association with appetite-regulating hormones, including GLP-1. These foods contribute to feelings of fullness and may support steadier post-meal glucose responses as part of a balanced diet.
Research exploring GLP-1 has primarily focused on its role in appetite regulation and glucose metabolism. While diet alone is not a treatment for metabolic conditions, nutritional approaches that prioritise whole, fibre-rich, and protein-containing foods are widely recommended to support long-term health. Individual responses can vary, and dietary strategies are most effective when tailored to personal needs, preferences, and medical guidance.
For those exploring structured weight-management support, clinically supervised programmes can help integrate nutrition, lifestyle, and medical considerations in a safe and evidence-informed way.
If you would like to learn more about medically supported weight-management options, SheMed offers personalised programmes designed to align with individual health goals. Eligibility assessment is available online to help determine whether a programme may be suitable.
References
- Holst, J. J. (2007). The physiology of glucagon-like peptide 1. Physiological Reviews, 87(4), 1409-1439. https://doi.org/10.1152/physrev.00034.2006
- Ratliff J, Leite JO, de Ogburn R, Puglisi MJ, VanHeest J, Fernandez ML. Consuming eggs for breakfast influences plasma glucose and ghrelin, while reducing energy intake during the next 24 hours in adult men. Nutrition Research. 2010 Feb 1;30(2):96-103.https://www.sciencedirect.com/science/article/abs/pii/S0271531710000035
- Li TY, Brennan AM, Wedick NM, Mantzoros C, Rifai N, Hu FB. Regular consumption of nuts is associated with a lower risk of cardiovascular disease in women with type 2 diabetes. The Journal of Nutrition. 2009 Jul 1;139(7):1333-8.https://www.sciencedirect.com/science/article/pii/S00223166
- Esposito K, Maiorino MI, Ciotola M, et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomised trial. Ann Intern Med. 2009;151(5):306-314. doi:10.7326/0003-4819-151-5-200909010-00004.
- Indarto D, Rochmah DN, Wiboworini B, Pratama YM, Wibowo YC. Effects of Vegetables Consumption Before Carbohydrates on Blood Glucose and GLP-1 Levels Among Diabetic Patients in Indonesia. Int J Prev Med. 2022;13:144. Published 2022 Nov 23. doi:10.4103/ijpvm.IJPVM_704_20